Stroke and Traumatic CNS injury
Stroke
Ischemic stroke is the most frequent cause of persistent neurological disability and, together with myocardial infarction, the most important reason for vascular death in modern western societies. Therapeutic intervention via systemic or local thrombolysis is currently only possible in a narrow time window of 3-6 hours after stroke. However, a large body of evidence suggests that stroke-induced brain damage progresses during subacute stages after the insult, causing delayed expansion of the infarctions along with clinical worsening or impaired recovery. Thus, there is an urgent need for new therapeutic strategies that could be applied in later stages of ischemic lesion development. Stroke research at our institution encompasses both experimental and clinical approaches to stroke pathogenesis, therapy, prevention, as well as regeneration.
Traumatic CNS injury
Traumatic brain and spinal cord injury (SCI) have devastating personal consequences for these patients and their families. Unfortunately, there is still no cure available. In addition there are enormous socio-economic costs ranging from 1-2 Mrd Euro every year in Germany (30-40.000 SCI patients).
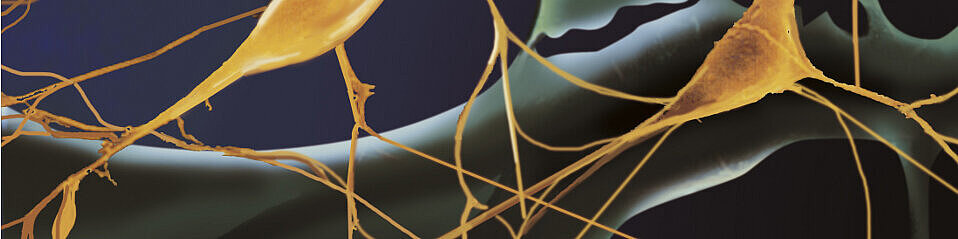
In contrast to the peripheral nervous system (PNS) where spontaneous axonal regeneration occurs, interrupted neuronal fiber tracts in the central nervous system (CNS) do not restore in adult mammals. Although lesioned CNS axons are capable to regrow in a favorable environment such as PNS tissue implants, they do not spontaneously regenerate within the CNS tissue. At least they do not extend far enough to reestablish lost functional connections with their original targets. The reason for this inherent difference of CNS versus PNS neurons might be due to the interplay between the following factors: (a) deficits in intrinsic neuronal capacities to start a regeneration program after lesion, (b) lack of growth support, for example, of neurotrophic factors, (c) suppression of axonal outgrowth by inhibitory molecules present in the environment. Moreover, some neuronal subpopulations of the CNS might respond more rigorously to distinct inhibitory molecules than others.
Research in this clinically relevant field is dedicated to the investigation of the suppression of regeneration barriers in the CNS, analysis and understanding of the molecular regeneration program of neurons, identification of regulatory signalling pathways underlying neuronal repair, mechanisms to support neuronal maintenance and protection after injury with the aim to develop and validate novel therapeutic concepts for translation into clinical application. These topics are experimentally addressed in different CNS lesion model systems and treatment paradigms.
PIs
The lab of Hans Werner Müller has a track record in (i) pharmacological suppression of regeneration inhibitory lesion scarring (Klapka, Eur J Neurosci 2005), (ii) chemokine-mediated stimulation of axon growth (Opatz, Mol Cell Neurobiol 2009), (iii) significant clinical, neuropathological and behavioural recovery using well-defined somatic stem cell grafts from human cord blood (Schira, Brain 2011) as well as (iv) comparative transcriptomic analyses of the complex molecular regeneration programs in the CNS (sensory motor cortex) and PNS (sensory ganglia, spinal motoneurons) following injury and therapeutic treatment (Kruse, Front Mol Neurosci 2011).
Rüdiger J. Seitz who is head of the division of cognitive neurology has a long standing interest in the mechanisms of recovery from stroke using neuroimaging and neurophysiological methods. His work extends from clinical investigations on the effects of thrombolysis in the acute phase immediately to cerebral plasticity and cognitive training strategies in neurorehabilitation in the chronic stage after stroke (Seitz et al., Radiology 2005; Seitz et al., J Magnet Resonance Imaging 2010; Seitz et al., Cerebrovasc Dis 2011). Moreover, considering cell-based regeneration approaches for restorative stroke therapy, his group analyses which brain structures and cell types are candidates for substitution and how new neuronal functionality could be implemented in a damaged brain by capitalizing on current concepts of post stroke plasticity (Dihné et al., Stroke 2011).