Hepatic encephalopathy
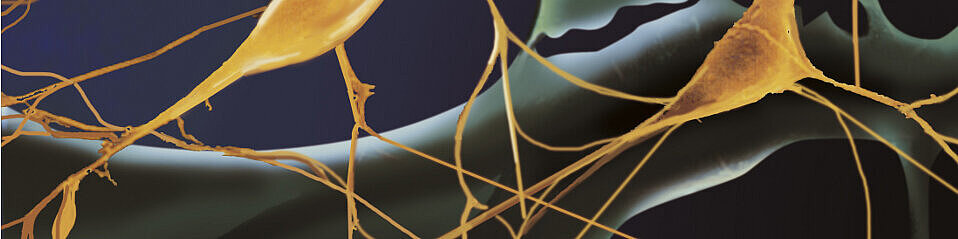
Hepatic encephalopathy (HE) is a serious neuropsychiatric complication of acute or chronic liver failure. The pathophysiological mechanisms are not fully understood, but ammonia, normally detoxified in the liver, accumulates in blood and brain and plays a key role in the pathogenesis of HE. Consequences of ammonia toxicity that preferentially affect astrocytes are astrocyte swelling with disturbance of brain water homeostasis and the development of low grade cerebral oedema, oxidative/nitrosative stress response, RNA oxidation and protein modifications, altered intracellular signalling, imbalance of neurotransmitter systems, disturbed expression of receptors, impaired synaptic plasticity and disturbances of oscillatory cerebral networks. In addition to ammonia, further pathogenic factors include inflammatory cytokines and neurosteroids that enhance the GABAergic tone and worsen clinical symptoms.
Investigations of pathogenetic and pathophysiologic mechanisms of HE have been major research focuses in the collaborative research centre 575 and the newly granted CRC 974 both coordinated by Dieter Häussinger. Research projects range from subcellular molecular approaches in vitro to non-invasive systems level analysis of human brain function in HE patients.
PIs
Orhan Aktas is interested in the impact of metabolic and inflammatory mechanisms on brain protein homeostasis in the course of liver failure. In HE, direct correlation of clinical symptoms with primary metabolic alterations is often weak, suggesting mechanisms of disease beyond elevated ammonia concentrations. Minute innate inflammatory challenges, e.g. low-level endotoxemia occurring in the course of liver failure, may additionally contribute to manifestation of HE and brain damage. Based on promising findings suggesting the involvement of the inducible proteosome. O. Aktas is investigating these processes in collaboration with O. Sergeeva and N. Klöcker.
Boris Görg investigates consequences of ammonia-induced astrocyte swelling on intracellular and intercellular signaling (Haussinger, Curr Opin Clin Nutr 2010). Based on cell biological studies, the group has developed a model of HE, in which ammonia and other precipitating factors such as pro-inflammatory cytokines trigger astrocytic swelling. This results in multiple alterations of astrocyte function and gene expression, in part through oxidative stress-dependent modifications of proteins and RNA.
Oxidative stress also affects glioneuronal communication and induces RNA oxidation in astrocytes and neurons with impact on synaptic plasticity and oscillatory network activity. Future studies will focus on the relationship between oxidative and volume stress in astrocytes neurons and microglia, as well as on the consequences of ammonia-induced RNA oxidation for expression and function ofgene products in vivo and in vitro.
The role of bile acid receptor TGR5, which acts as a neurosteroid receptor and has only recently been identified onastrocytes, neurons and microglia (Keitel, Glia 2010), will be explored. Moreover, the question will be addressed whether or not other metabolic encephalopathies caused by uremia, hypercalcemia, hypernatremia or thyreotoxicosis share pathophysiological mechanisms of HE.
Nikolaj Klöcker studies the molecular composition of AMPA-receptors by employing a functional proteomics approach (Schulte, Neuron 2006; Schwenk, Science 2009; Zolles, Neuron 2009; Schwenk, Neuron 2012) and uses cell biological as well as electrophysiological investigations to characterize the functional significance of identified complex constituents. Initial experiments demonstrate differential regulation of selected receptor complex constituents in HE, thus differential proteome analysis of AMPA receptors (HE vs. healthy control) will be used to elucidate the molecular basis of the alterations in glutamatergic neurotransmission in HE (Schroeter, MCN 2015).
Christine R. Rose studies mechanisms of cellular ammonia influx into astrocytes and neurons of hippocampal slices (Kelly, Glia 2009).
Alfons Schnitzler applies whole-head magnetoencephalography together with MRI and TMS to noninvasively study oscillatory networks in the human brain (Schnitzler, Nat Rev Neurosci 2005). His group has identified distinct disturbances of motor and attention-related oscillatory brain networks as the common pathophysiological pathway underlying diverse motor ans cognitive symptoms in HE (Timmermann, Clin Neurophysiol 2008). Future studies will investigate how these network disturbances are related to the pathomechanisms of HE studied. Brain network analysis will be combined with quantitative brain water imaging, GABA and glutamate spectroscopy, TMS, and pharmacological challenge of the GABA(A) receptor. MEG brain network analyses will be extended to the study of resting-state MRI networks in HE, which will be recorded simultaneously with metabolic brain activity and GABAA-receptor function (Flumazenil-PET) using a state-of-the-art hybrid MRI-PET system available at the FZJ. Furthermore, the question will be addressed whether pathophysiological mechanisms of HE are distinct from or shared by other types of metabolic encephalopathies.